Chronic Venous Insufficiency (CVI) is a condition that affects millions worldwide, often causing discomfort and potential complications if left untreated. Understanding the risk factors associated with CVI is crucial for early detection, prevention, and effective management.
In this comprehensive guide, we delve into the key risk factors contributing to CVI and explore how individuals can mitigate these risks.
What is Chronic Venous Insufficiency?
Chronic Venous Insufficiency occurs when the veins in the legs fail to efficiently return blood to the heart. Normally, one-way valves in the veins keep blood flowing upward toward the heart against gravity. When these valves become weakened or damaged, blood can pool or flow backward (reflux), leading to CVI. This condition can cause symptoms such as swelling, pain, skin changes, and in severe cases, ulcers.
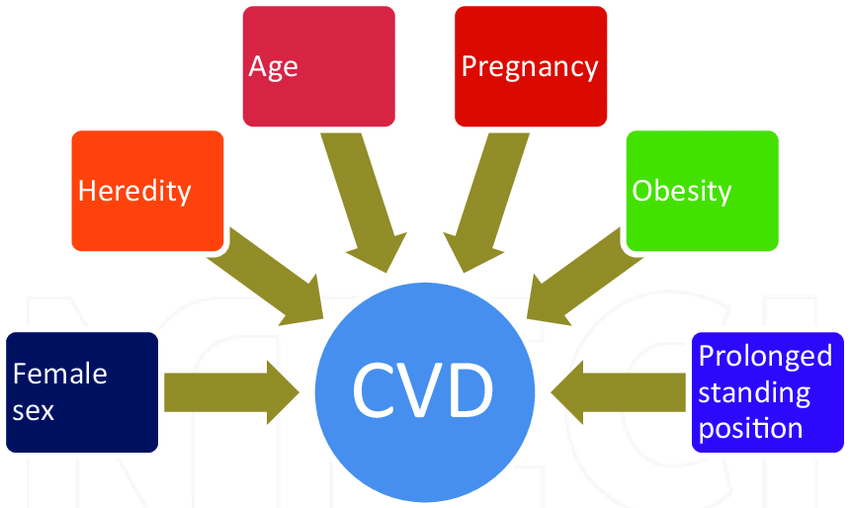
Risk Factors for Chronic Venous Insufficiency
Several factors contribute to the development of CVI. While some are unavoidable, others can be managed through lifestyle changes and medical intervention:
Age:
Advancing age is a significant risk factor for CVI. As people get older, the veins can lose elasticity and the valves may weaken, making it harder for blood to flow efficiently.
Gender:
Women are more likely to develop CVI than men. Hormonal changes during pregnancy, menopause, and the use of hormonal birth control can increase the risk.
Family History:
A family history of venous diseases, such as varicose veins or deep vein thrombosis (DVT), increases the likelihood of developing CVI. Genetic predisposition plays a role in weakening vein walls and valves.
Obesity:
Excess weight puts added pressure on the veins, particularly those in the legs, impairing circulation and increasing the risk of CVI.
Sedentary Lifestyle:
Lack of physical activity can lead to poor circulation and weaken vein walls over time. Regular exercise helps maintain healthy blood flow and strengthens the muscles that support veins.
Occupational Factors:
Jobs that require prolonged periods of standing or sitting can strain the veins and contribute to CVI. Examples include nurses, teachers, factory workers, and office professionals.
Smoking:
Tobacco use can damage blood vessels and impair circulation, making individuals more susceptible to CVI and other cardiovascular conditions.
History of Blood Clots:
Previous episodes of deep vein thrombosis (DVT) or blood clots in the legs can damage veins and valves, increasing the risk of CVI.
Pregnancy:
Pregnancy increases pressure on the veins in the legs due to the growing uterus. Hormonal changes and increased blood volume can also weaken vein walls and valves, leading to CVI.
Other Medical Conditions:
Certain conditions, such as high blood pressure (hypertension) and chronic heart disease, can affect blood flow and contribute to venous insufficiency.
Preventive Measures and Lifestyle Modifications
While some risk factors like age and family history cannot be changed, several strategies can help reduce the risk of developing or worsening CVI:
Maintain a Healthy Weight: Losing excess weight reduces pressure on the veins and improves overall circulation.
Stay Active: Engage in regular physical activity to promote circulation and strengthen leg muscles. Activities such as walking, swimming, and cycling are beneficial.
Avoid Prolonged Sitting or Standing: Take breaks to move around and stretch if your job involves long periods of sitting or standing.
Elevate Your Legs: Elevate your legs above heart level when resting to reduce swelling and improve blood flow.
Wear Compression Stockings: Compression stockings provide graduated pressure to support veins and help blood flow more efficiently.
Quit Smoking: Quitting smoking improves overall cardiovascular health and reduces the risk of venous insufficiency.
Manage Existing Conditions: Control conditions like hypertension and diabetes through lifestyle changes and medication to minimize their impact on vein health.
Seeking Medical Advice
If you notice symptoms such as leg pain, swelling, varicose veins, or changes in skin texture, it is important to seek prompt medical attention. Consulting a healthcare professional early on can lead to timely diagnosis and treatment, which are crucial in preventing complications and enhancing quality of life.
In Tulsa, options such as sclerotherapy can be explored to address these symptoms effectively and improve vein health. Taking proactive steps towards diagnosis and treatment ensures better management of conditions like Chronic Venous Insufficiency, promoting overall well-being and reducing the impact on daily life.
Conclusion
Understanding the risk factors associated with Chronic Venous Insufficiency empowers individuals to take proactive steps toward prevention and management. By adopting a healthy lifestyle, addressing modifiable risk factors, and seeking medical advice when needed, individuals can reduce the impact of CVI on their daily lives and overall health.
Incorporating these strategies can promote better vein health and contribute to a higher quality of life for those at risk of or living with Chronic Venous Insufficiency.